What are the primary drivers of unused capacity?
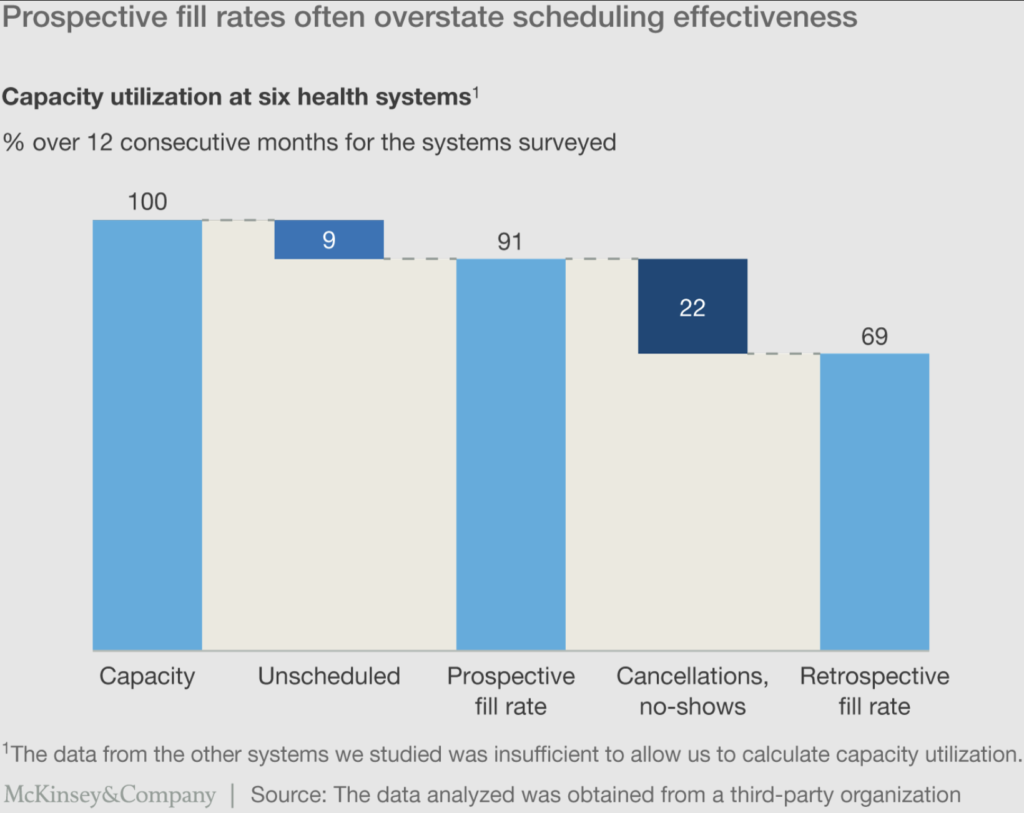
Scheduling into slots was the first problem we examined. After analyzing data from the first six systems for which we had complete prospective and retrospective fill rates for all physicians and clinics, we found that unscheduled slots accounted for almost 10% of the gap to full capacity (Exhibit 2).11 We then identified a difference between prospective and retrospective fill rates of around 20%, a result of cancellations with greater than 24 hours’ notice that were not backfilled, late cancellations, and no-shows.
Exhibit 2
How does utilization vary for specialties within the physician organizations?
Variability in retrospective fill rates exists not only across health systems, but also within physician organizations at the specialty level. Among the systems for which we mapped variations by specialty, we observed significant disparities—differences between specialties as high as 20%—even among the physician organizations with retrospective fill rates near the median overall (Exhibit 3). This variation underscores the importance of disaggregating performance at the physician or clinic level to analyze performance factors, including schedule templates and panel sizes (which tend to be physician-driven) and scheduling turnover (which tends to be clinic-driven), to identify root causes and propose solutions.
Exhibit 3

Improving front-door access is an essential part of an integrated growth strategy, especially given the imperative for health systems to expand both their share of lives and share of wallet among consumers ages 45 to 64 with commercial insurance. Among consumers with chronic disease in this demographic group, more than 90% of the value of inpatient and hospital-based outpatient claims are, on average, with a single health system.12 Providing access to consumers as they seek it will be essential to compete early on for these consumers and to attach them to the health system for the long term.
Impact of patient access performance on health system economics
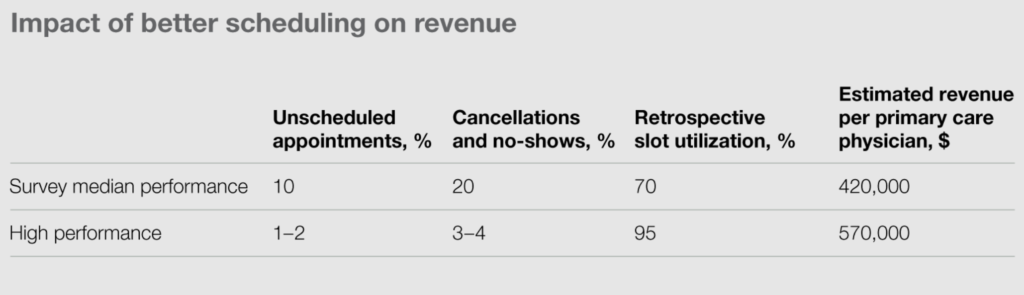
As we discuss in the main article, improving patient access can strengthen care delivery, increase patient satisfaction, and enhance patients’ health. Improving access also has bottom-line impact: improving health system economics. To understand its potential impact, consider these illustrative calculations:
Potential revenue per primary care physician
Total revenue per primary care appointment. . . . . . . . . $125
X
Number of appointments per day. . . . . . . . . . . . . . . . . 20
X
Numbers of days worked per year. . . . . . . . . . . . . . . . . 240
=
Potential revenue per primary care physician . . . . . . . . $600,000
Implications
- Closing half the gap between median and high performance on retrospective slot utilization would equate to an additional 600 visits—and $75,000 in direct revenue—annually
- The additional visits have the potential to enable better care coordination via referrals to aligned specialists and facilities
- Given that family physicians and internists generate, on average, $1.5 million to $1.8 million in net revenue for affiliated hospitals, the additional visits could bring in as much as $300,000 in indirect revenue1
Exhibit 4
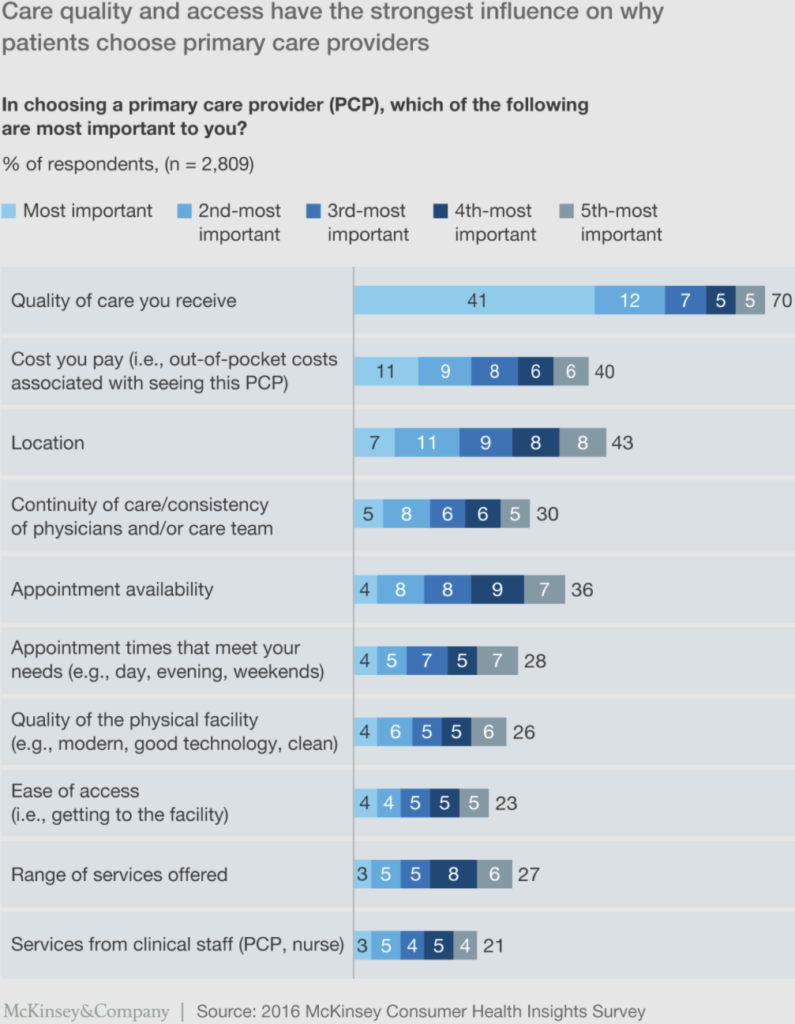
What do patients want
Desire for appointment availability. When asked to select the criteria that matter most to them when choosing a primary care provider, respondents highlighted “appointment availability” and “appointment times that meet your needs” as two of the top six factors, among 20 available options (Exhibit 4).
Booking. While 75% said they had attempted to book an appointment, only 57% were able to do so. Among those who did book appointments, the majority (68%) did so via phone; only 14% were able to book online. (The remaining 12% booked in person.)
Convenience. Three-quarters of those who booked appointments were able to get a convenient time; the other quarter were unable to do so, usually because it took “too long to get an appointment.” Among those able to book appointments, about one-quarter reported that weekend and evening slots were available; another 10% reported either weekends-only or evenings-only availability. The remainder said that their primary care practices offered neither weekend nor evening appointments.
Time to appointment. Nearly 70% of the respondents who booked an appointment for primary care got one within two weeks, with just over 30% given an appointment within one week (Exhibit 5).
Exhibit 6
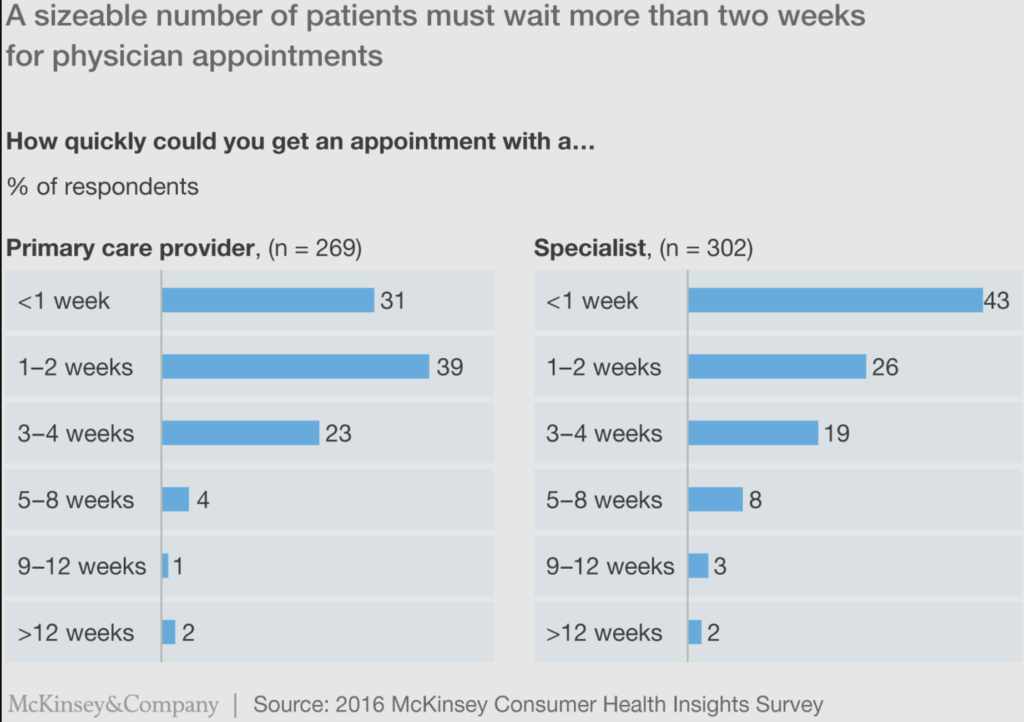
This means your medical spa (likely unlike the nearest dermatologist)should have a mere 1-2 week wait time.
Approach for moving forward
Addressing physician practices’ performance requires an end-to-end view that integrates physician preferences, best practices in clinical-level operations and consumer engagement, and central service infrastructure (e.g., technology platforms, call centers). It also requires setting a high bar and aligning the culture behind devotion to a consumer-first service mind-set. Our recent experience suggests that there are four key dimensions to transforming practice performance:
Introducing standards, tools, and capabilities
Many health systems invested capital to acquire practices, then under-invested in the time and resources required to integrate these acquisitions and enable high performance. As the number of employed-physician practices expanded and more new providers were hired, systems have often been left with myriad software solutions, policies, procedures, and norms for practice performance. In recent years, many health systems have started—and continue—to integrate and standardize operations, with a focus on:
Schedule template standardization, including setting best-practice appointment lengths, eliminating discretionary blocked time, and defining an approach to double-booking (to remove this decision authority from the individual clinic-level operators).
Call center optimization, including introducing single call numbers, reducing hold times, adding interactive voice responses, and improving staff scripting.
Third-party scheduling integration, for example, by using Zocdoc, Amion, QGenda, or Clockwise.MD, as well as by using automated appointment reminder tools, such as text messaging solutions.
Standardization and transparency into appointment availability support both call center and third-party scheduling because it enables those channels, separate from the individual clinics, to book appointments. Engaging these channels opens the front door wider for consumers, but implementing their use is no small matter; it can take large health systems as long as 12 to 18 months, depending on their starting points.
Supportive changes—such as having providers practice at the top of their licenses, setting standards for which providers see different types of patients, and enhancing collaboration between the clinics and call center and IT support teams—often also need to be undertaken in tandem with schedule optimization. The operational and cultural changes required to achieve all these goals speak to why change often requires patience and time to materialize.
Establishing ongoing performance management
Executing and sustaining a clinic-level transformation requires strong performance management enabled by real-time data. We have often found that physicians and clinic staff working in a practice purchased by a health system operate as though they were still in an independent practice—without sharing data or interfacing regularly with the health system. Key elements needed to implement strong performance management include:
Defining the metrics to track. As few as possible should be used, and the selected metrics should be those best tied to the system’s desired outcomes. In our experience, the set of metrics should include specific measures of productivity (e.g., total wRVUs, out-of-network referrals) and scheduling (e.g., retrospective fill rate, short-notice and no-show cancellations), as well as assessments of patient satisfaction, revenue cycle results, and new physician ramp-up performance. Some health systems focusing on the financial implications of low productivity have even quantified the opportunity (in terms of the number of additional wRVUs or the anticipated increases in revenues) to highlight the gap between current performance and their goals. The selected set should enable both the system and any practice being studied for acquisition to establish baseline performance (especially on key metrics) and to agree on targets, ideally based on comparisons with internal and peer benchmarks.
Supplying useful data to advise the clinic teams’ decisions. In addition to selecting metrics, the health system and practice need to create processes for data collection and sharing. Reporting should be done on a daily and/or real-time basis. At a minimum, each clinic should have visibility into its own performance and, for comparison, the system’s aggregate performance or, perhaps, other individual clinics’ performance. The full clinic staff, not only its leadership, need to be able to access and understand the data.
Developing a governance and operating cadence in the clinics. The basic infrastructure should include huddles that cascade from the front-line clinic teams to physician organization leadership. For large systems, the best practices we have observed involve:
- Daily huddles around metrics in each clinic
- Weekly problem-solving sessions with front-line teams and clinic managers to address ongoing issues
- Weekly leadership meetings in which all clinic leaders and the physician organization management team review changes in key performance indicators and offer support to solve issues raised by the front-line teams
Improving practice leadership and operating models
Until recently, many individual and small group physician practices sustained themselves as small businesses. Upon joining large employed groups, the physicians and clinic staff often fail to adapt their operating models. This cannot continue. For many health systems, large employed-physician organizations now represent business units with hundreds, if not thousands, of employees and revenue figures above $500 million annually. Thus, when health systems bring the physicians and clinic staff on board, it is crucial that they set appropriate expecations—and health system leaders must be more direct than ever before.
For example, improving consumer satisfaction may require offering evening and weekend appointments, and physicians may have to accept that their incentives will be based on reported consumer satisfaction, not just productivity. In addition, physicians and clinic staff should expect to work in pods with expanded panel sizes, with an understanding that each clinic will operate as a team. The practices will need to hold individual providers accountable for any failure to respect patients as consumers (e.g., by arriving late to appointments) and to promote the effective use of scheduling technologies—and other new technologies—deployed across the system. Health system leaders may even consider introducing individuals from consumer-oriented industries into clinic staff and practice leadership roles to help accelerate the culture changes often required.
Managing referrals to support care continuity and productivity
As health systems resolve operational challenges around access, other issues must be addressed to realize the full potential from the improvements. One is referral management. Many systems continue to see significant out-of-network referrals from employed-physician practices to independent physicians or competitors, even when they have appropriate providers for the services required. Often, the referring physicians cite scheduling delays as the proximate cause; however, lack of awareness of and relationships with their peers within the system is often the root cause. Engaging a health system’s physician relationship management function can help. In addition, analyzing referral data for the sources of leakage—especially between primary care and specialists—and then being prepared to propose alternatives can drive behavioral change. Communicating expectations to the specialist clinics, including the need to send patients and information back to the referring primary care provider, is also critical.
Additional functions within health systems can also help support productivity improvements. For example, digital marketing teams can make consumers aware of physicians once those with sufficient capacity have been identified. Continuity of care efforts can also help. For instance, patients who visit the emergency department who need a specialist follow-up or who do not have a primary care provider can be given appointments with employed physicians, an approach that not only improves productivity but also addresses patients’ needs and ensures more integrated care.
As these activities suggest, significant blocking and tackling are often required—across people, processes, and technology—to optimize practice operations. The difficulties involved explain, in part, why some health systems see lagging results and underscore the value for those that succeed.
Defining the metrics used to assess physician utilization
Appointment cancellation rate: Total appointments cancelled divided by total appointments booked per physician FTE; can be as high as 30% for large groups
Capacity: Contracted hours per physician FTE (excludes administrative time, vacation, teaching time, etc.)
No-show rate: Non-cancelled appointments when the patient did not appear for appointment divided by total non-cancelled appointments per physician FTE; can be as high as 20% for large groups
Prospective fill rate: Scheduled appointment hours divided by contracted hours per physician FTE
Retrospective fill rate: Total hours with completed appointments divided by the total contracted hours of physician capacity; can be 20% to 30% lower than prospective fill rate for large groups
Short-notice cancellation rate: Appointments cancelled within 24 hours of scheduled appointment divided by total appointments booked per physician FTE; can be as high as 15% for large groups
* * *
In recent years, many health systems have employed significantly more physicians, especially primary care providers, to improve care coordination. Too often, however, the acquired practices have not evolved from small businesses to professionally scaled, customer-centric enterprises. As a result, productivity has declined, operations have not improved, and access remains a challenge. Solutions relying on training more physicians could take a decade to affect patient access, and policy changes to expand mid-level providers’ scope of practice face legislative hurdles. Therefore, maximizing the operating efficiency of large employed-physician organizations is an urgent need if health systems are to meet their dual goals of improving patient access and financial performance. Systems that succeed in making this transition, and quickly, can expect to win consumers and engage with them effectively, aligning them closely with their physicians—and the health system.
What is clinical operations excellence?
Clinical operations excellence includes elements of traditional hospital performance improvement efforts (especially lean transformations), but it goes beyond them because of the emphasis it places on improving care delivery as well as nonclinical operations (Exhibit 1). It uses a variety of process improvement and change management concepts and approaches to increase operational efficiency and reduce clinical variability; the ultimate objective is to drive down the total cost of care while maintaining or improving care quality.
In our experience, most hospitals have significant, unintentional variability in how clinical care is delivered. Most hospital executives would agree that this variability drives up the cost of care, making hospitals less competitive and less likely to survive in a world of value-based payment. Reducing clinical variability would release working capital (e.g., through inventory reduction), lower supply costs (e.g., by shifting to one or two vendors), increase the pace of care delivery (e.g., by reducing the number of potential paths of care), shorten average length of stay (e.g., by initiating care sooner in the care pathway), and reduce the likelihood of adverse events (e.g., by standardizing and error-proofing nursing workflows).
Physicians can be convinced to reduce the amount of variability in care delivery if they understand that the changes will not only help control costs but also improve patient outcomes. By ensuring that all patients receive high-quality care in a reproducible and evidence-driven manner, a virtuous circle can be created: as the quality and efficiency of care delivery rise, per-patient costs decrease, outcomes improve, patient and staff satisfaction increase, referral streams expand, and high-volume physicians become less likely to migrate to other hospitals.
Implementing the changes necessary to reduce or eliminate unintentional variability in care delivery in a sustainable way is far from easy. It requires a complex combination of approaches to streamline processes (including those for patient admissions and discharges), standardize clinical protocols, and rationalize supply utilization. Our experience suggests, however, that this combination can have a significant impact (Exhibit 2).
After using this multiprong approach in more than 150 hospital transformations over the past few years, we have found that it can significantly improve hospital performance. On average, most hospitals see a reduction of 5 percent or more in operating costs (Exhibit 3).
How to Raise Utilization Rates
To raise an organization’s capacity utilization rate, you need to increase all of its employee utilization rates, since capacity is an average of the individuals.
A good first step is to set baselines for each employee, as we discussed earlier. If you remember, Leslie’s utilization is 75%, which allows her some time for non-billable administrative work.
It’s vital that you share these target utilization rates with each employee and their managers. It’s impossible to hit a target if you don’t know what you’re shooting for. Allow employees to take ownership of their utilization rate, and don’t punish employees who don’t hit their target rate (unless it’s because of negligence). It’s probably not their fault if there isn’t enough billable work to charge for.
Instead, reward employees who manage to hit or exceed their utilization targets. Employees who are positively motivated to hit their goals will take a more active role in the company. They may even go so far as to try and bring in business to boost billable hours. Ideally, your employees should see target utilization rates as an exciting challenge, not a weight on their shoulders.
Use Time Tracking Software
There are plenty of benefits to using time tracking software to track billable hours, as long as the tool is easy to use. It’s possible that your employees are already billing at higher rates, but because time tracking is such a hassle, they either aren’t adequately or accurately billing all of their hours. Or perhaps some of their hours are getting miscategorized because of poor software design and implementation.
Time tracking software ideally makes the process as easy and as accurate as possible. Once your employees start accurately recording their hours in a timely fashion, you may discover that your organization is doing better than you thought.
Minimize Non-Billable Time
This is a big one. As we said, every company needs some non-billable time built into its schedule, but too much non-billable time is an indication of waste. This can be an indication that:
- You don’t have enough billable work to fill your pipeline, and employees are twiddling their thumbs
- There are inefficiencies in internal processes that are causing excess administrative time
- Managers need to get back in the trenches and take on more billable work
- Available training time isn’t adequately preparing junior team members to handle the available workload
We already know that available time is a finite resource. If too much of it is getting sucked up by non-billable, administrative work, it skews your team’s availability, distorting perception of the number of hours that could be devoted to paying work.
This can lead to disastrous consequences, like being turned down for a perceived lack of capacity to do the work, and further degrading the backlog of billable work that could raise your utilization rates.
From that perspective, reducing wasted non-billable hours can create a positive feedback loop that ramps utilization rates in an upward trajectory.
Lessons from other industries
In other industries, high customer satisfaction levels have been linked with stronger loyalty, sales, and profits. McKinsey research in multiple industries has shown that companies that routinely achieve high customer satisfaction scores rely on best-practice measurement systems that:
- Link improvements in the customer experience with desired business outcomes (e.g., repeat sales)
- Enable the companies to identify the most important drivers of customer satisfaction and measure ongoing performance in those areas
- Uncover operational insights that enable the frontline staff to make continuous improvements in the customer experience
Applying these lessons in health systems
To date, few health systems have achieved significant business results through patient-experience initiatives. Yet, growing consumerism in the healthcare industry—a result of higher deductibles and copayments, network narrowing, and greater transparency into provider performance and costs—is likely to make patient-experience initiatives more of an imperative for the industry. The proliferation of provider-led health plans is also making it increasingly important for health systems to market themselves, and patient satisfaction could be a key differentiator in their marketing efforts.
The steps outlined below can enable providers to adapt best practices from other industries to the healthcare environment.
Link patient satisfaction to business outcomes
The first step for health systems is to determine the business outcomes they most want to focus on (e.g., total patient volume, patient retention, percentage of commercial patients). They should then conduct research to investigate the types of questions that will best enable them to gauge patient satisfaction in a way that ties into those objectives. For example, a major US health insurer discovered that customer agreement with the phrase “[company name] is the insurer for me” predicted loyalty in one of its most important member segments better than agreement with any other phrase did. Because member retention in that segment was one of its business objectives, the insurer then focused its efforts on how to increase the percentage of people in that segment who agreed with the phrase.
Next, health systems should conduct additional research to identify the factors that most strongly influence how patients respond to the chosen questions and the specific metrics that would enable them to assess performance in those areas. Over time, the combined data should permit the health systems to develop robust measurement systems that can uncover operational insights and enable continuous frontline improvements. To ensure that the measurement systems remain robust, health systems should repeat this fundamental research every few years so that their understanding of the patient experience is always current.
Identify the strongest influences on patient satisfaction
To determine which factors most strongly influence patient satisfaction, health systems must accurately understand the end-to-end inpatient journey, from pre-admission scheduling and testing through to follow-up care, as well as the role that price, service offerings, physician referrals, and brand play in determining where patients seek care (Exhibit 1).
Sources
McKinsey
