Noncore doctors – blog post
During its early years, the medical aesthetics industry was dominated by the physicians who are referred to as “core doctors”—plastic surgeons, ENT doctors, and dermatologists. This makes sense, since these physicians are well-suited to oversee and provide medical aesthetic services. However, in more recent years, more and more non-core doctors have entered the marketplace. Today, approximately 60% of all medical directors at medical spas are non-core physicians, and it’s likely that percentage will only increase in coming years. An incredible influx of non-core doctors is coming into the marketplace, and it is very likely that their ranks will expand as the popularity of medical spas increases and the public becomes more aware of these businesses.
Most non-core physicians enter the MedSpa arena to boost their compensation, define their brands and be their own bosses, and they are taking over the industry, much to core doctors’ chagrin.
In certain ways, medical spas are partial substitutes for the services of the dermatologist or plastic surgeon.
Though there’s a national physician shortage in multiple specialities. In dermatology, the shortage is large, and the patient experience suffers. For out-of-pocket procedures, compromises in patient experience leads to substitution.
According to the consultants at Merritt Hawkins & Associates, the average wait time for a dermatologist was 32.3 days.
Since all American doctors are licensed to perform surgery they are already trained, experienced, and competent in performing minor medical procedures. And that is exactly what a hair transplant is at its core: an in-office minor medical procedure. All they need is some basic training in how hair transplantation is actually done step by step and they should be able to start performing them.
legal risk of doing anything you are not trained for and clearly qualified to do is very great regardless of what diplomas may be are hanging on your wall.
Doctor must be trained and qualified in aesthetics – i.e. know counter indications
As medical director, I am responsible for the training or lack thereof of my employees
Before procedures, face-to-face or tele medical exam/consultation required – me, RN, or PA (you should consider making consults very affordable, or even free during your first year )
MED SCHOOL EQUIPMENT
Another major barrier to entry is the up-front investments that companies must make in management software, medical equipment and facilities necessary for a group of physicians.
***Many states have certificate-of-need (CON) regulations and other laws that limit the number of physician-owned medical facilities. Many CON laws were initially put into effect across the United States as part of the federal Health Planning Resources Development Act of 1974. Despite numerous changes over the past 30 years, 36 states retain some type of CON program, law or agency as of 2019 (latest data available). These laws, along with recent health reform regulations, encourage physicians to join or form medical group practices that are managed by the industry. *****
non-core doctors flood
General supervision means the service is furnished under the physician’s overall direction and control, but the physician’s presence is not required during the performance of the procedure. Under general supervision, the training of the non-physician personnel who actually perform the diagnostic procedure and maintain the necessary equipment and supplies, is the physician’s continuing responsibility.
Supervision, delegation and noncompliant ownership are among the hot button issues that can land physicians in big trouble in the medical spa business, according to attorney Renee E. Coover with ByrdAdatto, a law firm specializing in health care and business law.
Coover shares what she says are three high risk areas — supervision, delegation and noncompliant ownership structure — for physicians who own or are medical directors of med spas, and how they can avoid potentially career-damaging liability outcomes.
Supervision and Delegation
Coover highlights two aspects of physician supervision and delegation at med spas. The first, she says, often has to do with noncore cosmetic doctors, including OB/GYNs, emergency room physicians and pediatricians, who become med spa directors or own these facilities.
The problem occurs when these doctors don’t have experience in medical aesthetic treatment.
“To be a supervisor or medical director of a medical spa, it’s really important that the physicians, themselves, have the appropriate experience and training. At the end of the day, if the medical board opens an investigation based on a disgruntled patient, employee or even a vindictive ex-spouse, that physician has to be able to defend himself or herself in front of the medical board as to why certain treatments were performed in the ways that they were. If that physician doesn’t have appropriate training and experience in the medical treatments and services that are being offered at that medical spa, it is not appropriate for the physician to be supervising and delegating those treatments.”
4. Medi-spa staffs aren’t trained to spot cancer.
A pesky pimple or unsightly mole may be more than just a cosmetic concern. Board-certified dermatologists, plastic and facial plastic surgeons are trained to identify and remove potentially cancerous lesions—and send the tissue to an appropriate lab for diagnosis. An aesthetician with limited knowledge of skin lesions may miss this. This is why you could try to consult every patient that walks into your facility.. And give referrals to derms when needed
Cosmetic dermatological procedures represent the smallest service segment, although demand for such services has grown from the aging population.
Currently, cosmetic dermatological procedures are estimated to account for 10.0% of industry revenue in 2019, according to a survey published by the American Academy of Dermatology (AAD). Cosmetic dermatology procedures tend to be characterized by higher margins and include treatments such as Botox injections, liposuction and cosmetic laser treatments. these procedures are not commonly covered by health insurance plans. Therefore, demand tends to uctuate more in line with discretionary spending and disposable income since the majority of patients pay for such services out-of-pocket.
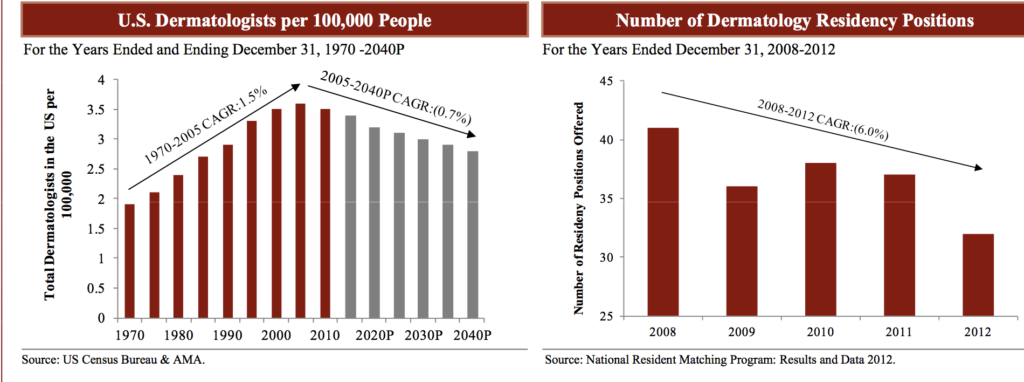
A physician’s training is costly. In fact, according to the Association of American Medical Colleges, more than 80.0% of medical school graduates are in debt for educational expenses. Even more than that, the number of dermatology residencies has not met the increased demand coming from the growing US population (yet alone meeting the demand coming from aging Baby Boomers).
READ ME
https://www.dermatologytimes.com/view/medical-spas-face-increasing-liability-risks
https://www.americanmedspa.org/news/412257/The-Rise-of-Non-Core-Doctors-and-What-It-Means.htm
https://modernaesthetics.com/articles/2018-july-aug/the-rise-of-non-core-doctors-and-what-it-means
